Understanding the Complex Relationship Between the Inner Ear and Balance
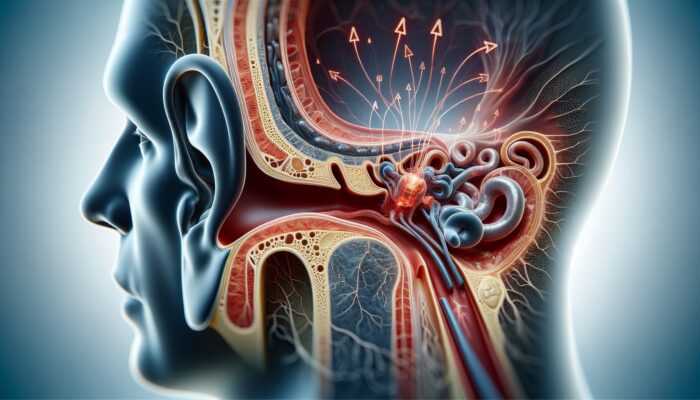
The inner ear is an extraordinary feat of biological engineering, intricately designed to play a crucial role in maintaining balance. Central to this system is the vestibular apparatus, which is essential for helping us navigate our surroundings with both stability and accuracy. When we explore how ear conditions affect balance, it’s vital to recognize the significant influence this system has on our daily activities and overall well-being. The ability to maintain equilibrium is foundational to performing everything from everyday tasks to more complex physical activities, and any disruption can have far-reaching consequences.
How the Vestibular System Guides Our Sense of Balance
The vestibular system comprises the semicircular canals and otolith organs, which collaborate seamlessly to detect head movements and positional changes in space. Each time we turn our heads, tilt, or shift our weight, these structures provide vital signals to the brain, contributing to our sense of balance. Think of them as a finely-tuned compass that continuously guides us through our environment. When functioning optimally, the vestibular system enables us to engage in activities as diverse as strolling through a bustling street in Tokyo or traversing the challenging trails of the Andes, all while maintaining our footing and orientation.
However, any disruptions within this system can lead to significant challenges in maintaining balance. Conditions like vestibular neuritis or BPPV (Benign Paroxysmal Positional Vertigo) can interfere with the transmission of these critical signals, resulting in feelings of disorientation and instability. This underscores the importance of understanding how ear conditions affect balance, as the manifestations can vary greatly, often appearing as dizziness or a spinning sensation, severely impacting one’s capability to perform daily tasks with confidence.
The Consequences of Ear Infections on Balance
Ear infections extend beyond being a typical childhood issue; they can have profound effects on balance and overall equilibrium. Infections affecting the middle or inner ear can lead to inflammation, disrupting the delicate balance regulated by the vestibular system. For example, a case of otitis media, which refers to an infection in the middle ear, can result in fluid buildup that alters pressure and impairs the function of the inner ear, leading to significant balance issues.
When this occurs, individuals may experience dizziness, a sensation of fullness in the ear, or even episodes of vertigo. These physical symptoms extend beyond mere discomfort; they can give rise to anxiety and avoidance behaviors, as the fear of losing balance may prevent individuals from participating in social activities or undertaking simple outings. As we delve into how ear conditions affect balance, it’s essential to acknowledge the psychological impact these physical sensations can impose on individuals, influencing their quality of life.
Moreover, the ramifications of ear infections can create a cyclical problem. Recurring infections can lead to cumulative damage to the vestibular system over time, exacerbating balance issues. This highlights the critical importance of timely diagnosis and treatment of ear infections—neglecting to address them can lead to chronic balance disorders that severely diminish one’s quality of life on a global scale.
Exploring the Effects of Meniere’s Disease on Balance
Meniere’s disease serves as a striking illustration of how a specific ear condition can result in significant balance disturbances. This condition is characterized by episodes of intense vertigo, often accompanied by fluctuating hearing loss and tinnitus. The suspected underlying cause is the accumulation of fluid within the inner ear, which disrupts pressure dynamics and directly affects the vestibular system’s functionality.
Those suffering from Meniere’s disease may find themselves confined to their homes during flare-ups, as the overwhelming nature of vertigo can be debilitating. This condition transcends geographical boundaries; people from various cultural backgrounds and climates—ranging from bustling urban centers in Europe to remote villages in Africa—experience its challenging effects.
The unpredictable episodes associated with Meniere’s disease emphasize the necessity of understanding how ear conditions affect balance. Such episodes can drastically alter daily routines, turning even mundane tasks like grocery shopping or commuting into daunting challenges. As the disease advances, the probability of falls increases, complicating the individual’s ability to partake in normal activities and maintain independence.
How Aging Affects Our Balance Mechanisms
As we advance in age, the vestibular system undergoes natural deterioration, which escalates the risk of balance disorders. This decline can be attributed to various physiological changes, including diminished function of the hair cells in the inner ear and a reduction in neural connections in the brain responsible for processing balance information. The implications of these changes can be profound for older adults, as they may struggle to maintain equilibrium and avoid falls.
Aging populations around the globe face significant challenges associated with balance and fall risks. For instance, older adults residing in urban areas may need to navigate uneven sidewalks or public transportation systems, while those living in rural settings may contend with natural terrain that heightens balance difficulties. The consequences of falls in this demographic can be severe, frequently resulting in hospitalizations and extended recovery periods.
Understanding how ear conditions affect balance empowers older adults and their caregivers to adopt proactive measures. Engaging in balance training exercises, scheduling regular check-ups, and implementing fall-proofing strategies in their living environments can significantly mitigate risks. Community programs that promote active lifestyles and foster social support can help reduce the negative impact of aging on balance, enabling individuals to maintain independence and enhance their quality of life.
Exploring Common Ear Conditions Impacting Balance
Investigating the wide array of ear conditions that can disrupt balance reveals a complex relationship between anatomy and functionality. Each condition presents unique challenges that necessitate specific diagnostic and treatment strategies, underscoring the importance of understanding how ear conditions affect balance.
Understanding Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is among the most prevalent vestibular disorders, characterized by brief, intense episodes of vertigo triggered by changes in head position. This condition occurs when tiny calcium carbonate crystals, known as otoconia, dislodge from their normal location in the utricle and migrate into one of the semicircular canals. This misplacement sends erroneous signals to the brain, inducing a spinning sensation that can be both disorienting and alarming.
Individuals with BPPV may find themselves experiencing dizziness while turning over in bed, looking upward, or bending down to pick something up. These episodes can be particularly disruptive, not only causing discomfort but also heightening the risk of falls. For instance, a person may feel stable while seated but find it difficult to navigate their surroundings when standing or moving quickly. Thus, BPPV exemplifies the significant impact that ear conditions can have on balance.
Treatment typically involves specific head maneuvers, such as the Epley maneuver, aimed at repositioning the otoconia to alleviate symptoms. Education regarding the condition is also critical; understanding that BPPV is often benign can help reduce the anxiety associated with episodes. Raising awareness of BPPV in a global context can empower individuals, regardless of location, to seek appropriate treatment and support.
Labyrinthitis and Vestibular Neuritis: Inflammation and Balance Disturbances
Labyrinthitis and vestibular neuritis are conditions that involve inflammation of the inner ear structures, leading to severe dizziness and balance disturbances. Labyrinthitis affects both auditory and vestibular functions, often stemming from a viral infection or, less frequently, a bacterial infection. Conversely, vestibular neuritis specifically targets the vestibular nerve, frequently triggered by viral illnesses such as the flu.
Both conditions can result in sudden and intense dizziness, leading to nausea and an inability to maintain balance. Imagine a traveler who arrives in a new city, eager to explore, only to be overwhelmed by a surge of dizziness that leaves them unable to move. This scenario is common for those affected by these conditions and can severely limit their ability to enjoy life.
The global perspective on labyrinthitis and vestibular neuritis shows that they can manifest anywhere, regardless of healthcare access or geographic location. Treatment generally involves medications to manage symptoms and vestibular rehabilitation therapy designed to enhance balance and facilitate recovery. Recognizing the signs and symptoms of these conditions can help individuals worldwide seek timely medical intervention, thereby reducing the long-term effects on their quality of life.
The Impact of Otosclerosis on Balance
Otosclerosis primarily affects the middle ear, leading to abnormal bone growth around the stapes bone, which can impede its ability to transmit sound vibrations effectively. While often recognized for its association with hearing loss, otosclerosis can also influence balance due to its effects on the structures of the inner ear.
As the condition progresses, individuals may start experiencing dizziness and a sense of unsteadiness, particularly in environments requiring quick adjustments to balance, such as busy markets or uneven trails. This is particularly relevant in regions where outdoor activities are integral to the culture, potentially limiting participation in social and recreational events.
Surgical intervention, typically a stapedectomy, can restore hearing and improve balance for many individuals. However, understanding how ear conditions affect balance is critical for those living with otosclerosis; early recognition of symptoms can facilitate better management strategies and enhance overall quality of life.
Identifying Symptoms of Balance Disorders
The symptoms of balance disorders associated with ear conditions can vary widely and are often complex to navigate. Recognizing these symptoms is the first step toward understanding the challenges faced by those affected and seeking appropriate help.
Experiencing Dizziness and Lightheadedness as Common Symptoms
Dizziness and lightheadedness are hallmark symptoms of balance disorders, particularly those related to ear conditions. For many individuals, these sensations can arise unexpectedly, creating a disorienting sense of instability. Picture yourself standing in a vibrant market in Marrakech, surrounded by colorful sights and sounds, only to be suddenly engulfed by dizziness that makes focusing or even standing upright difficult. This experience is not merely uncomfortable; it can lead to anxiety and a reluctance to engage in social situations.
Dizziness can manifest in various forms; some may describe it as faintness, while others may experience a spinning sensation known as vertigo. The psychological impact of these symptoms can be profound, as the fear of experiencing dizziness in public can lead to social isolation. This highlights the need for greater awareness and understanding of how ear conditions affect balance, fostering empathy and support within social circles.
Furthermore, the experience of lightheadedness can often be misinterpreted as unrelated health issues, resulting in misdiagnosis or delayed medical intervention. Education is crucial—understanding that these sensations may be linked to underlying ear conditions can prompt individuals to seek timely treatment, paving the way to improved balance and quality of life.
Vertigo and Nausea: A Debilitating Combination
Vertigo is a particularly incapacitating sensation that is frequently accompanied by nausea, creating a distressing cycle that can leave individuals feeling immobilized. Those who experience vertigo often describe it as a disorienting spinning sensation, as if the world around them is moving while they remain still. This can lead to significant distress, especially in unfamiliar environments or during daily activities such as commuting or driving.
Imagine a traveler exploring the ancient ruins of Machu Picchu, only to be suddenly overtaken by vertigo at high altitudes. Such incidents can force individuals to abandon their plans, negatively impacting not only their enjoyment but also their sense of independence and adventure. This scenario underscores the importance of understanding how ear conditions affect balance, particularly for those who thrive on mobility and exploration.
Addressing the symptoms of vertigo typically involves a combination of medical treatment and lifestyle adjustments. Patients may benefit from vestibular rehabilitation therapy, which is designed to help retrain the brain’s interpretation of balance signals. Additionally, being aware of potential triggers, such as sudden head movements or specific visual stimuli, can empower individuals to manage their conditions more effectively and maintain their quality of life.
Unsteadiness and the Fear of Falls
Unsteadiness is a common experience for those with balance disorders and is often accompanied by a heightened fear of falling. This fear can create a self-fulfilling prophecy; as individuals become more cautious, they may limit their mobility, leading to decreased physical fitness and increased frailty. This cycle can further perpetuate a decline in balance and stability, making engaging in everyday activities increasingly challenging.
In various settings worldwide—whether negotiating cobblestone streets in Europe or hiking through the hills of Southeast Asia—the risk of falls can be exacerbated by environmental factors. Poorly maintained sidewalks, uneven surfaces, and crowded areas can present significant hurdles for those grappling with balance issues.
Understanding how ear conditions affect balance can inform preventive strategies. Simple interventions, such as wearing supportive footwear, utilizing assistive devices, and implementing fall prevention measures in the home, can dramatically reduce the likelihood of falls. Community programs that promote physical activity and balance training can also create supportive environments, empowering individuals to regain confidence in their mobility.
Diagnosing Ear-Related Balance Issues Effectively
Diagnosing balance issues related to ear conditions requires a comprehensive approach, as their symptoms can often overlap with other medical concerns. A multifaceted assessment can unveil the underlying causes of balance disturbances, leading to more effective treatment strategies tailored to individual needs.
Significance of Hearing Tests in Diagnosis
Hearing tests are fundamental in diagnosing ear conditions that impact balance. Audiologists employ various techniques, such as pure-tone audiometry and speech recognition assessments, to evaluate an individual’s auditory capabilities. Changes in hearing frequently correlate with balance disorders, providing essential clues for accurate diagnosis.
For instance, a patient experiencing dizziness alongside hearing loss may be assessed for conditions such as Meniere’s disease or otosclerosis. Understanding the connection between hearing and balance is crucial, as it informs treatment decisions and enhances symptom management. On a global scale, access to hearing assessment services can vary widely, making it essential for communities to prioritize awareness and education about the importance of these tests.
Moreover, interpreting hearing test results can guide healthcare providers in determining the next steps for further evaluation. For example, abnormal hearing test outcomes may necessitate additional imaging studies or vestibular function tests to thoroughly explore the underlying causes of balance issues.
The Role of Vestibular Function Tests in Diagnosis
Vestibular function tests are critical for diagnosing balance disorders linked to ear conditions. These specialized assessments evaluate the vestibular system’s functioning, providing vital insights into how well the body maintains balance. Common tests include videonystagmography (VNG) and the vestibular evoked myogenic potential (VEMP) test, each designed to elicit specific responses from the vestibular system.
Through these tests, clinicians can identify abnormalities and dysfunctions in the vestibular pathways, aiding in the diagnosis of conditions such as vestibular neuritis or BPPV. By understanding how ear conditions affect balance, healthcare providers can customize their treatment approaches to address the unique needs of each patient effectively.
The global landscape of vestibular testing availability varies significantly. In urban areas, access to advanced diagnostic tools may be common, while individuals in remote or underserved regions may struggle to obtain these evaluations. Raising awareness about the importance of vestibular function testing can empower individuals globally to seek appropriate care and support for managing their balance disorders.
Imaging Studies and Other Diagnostic Tools
Imaging studies, including MRI or CT scans, can provide invaluable insights when diagnosing ear-related balance issues. These imaging tools offer a visual representation of the inner ear structures, revealing abnormalities that may contribute to balance disorders. For example, structural issues such as tumors or malformations may be identified using advanced imaging techniques.
In addition to imaging, other diagnostic methods, such as blood tests and comprehensive physical examinations, can help rule out potential causes of dizziness and balance problems. This comprehensive approach ensures that healthcare providers can arrive at an accurate diagnosis and implement appropriate treatment plans.
In regions with limited access to advanced diagnostic imaging, healthcare providers may rely on clinical evaluations and symptom assessments to guide their decision-making process. Recognizing the potential limitations of diagnostic resources worldwide emphasizes the need for ongoing advancements in medical technology and healthcare accessibility to benefit all patients.
By grasping how ear conditions affect balance, both patients and practitioners can collaborate effectively to navigate the complexities of diagnosis and treatment, ultimately working toward improved outcomes for individuals facing balance disorders.
Exploring Treatment Options for Balance Disorders
The landscape of treatment options for balance disorders stemming from ear conditions is diverse, ranging from medications to lifestyle changes. A comprehensive understanding of these options empowers individuals to make informed choices that can significantly enhance their quality of life.
Utilizing Medications and Therapies for Symptom Management
Medications are integral in managing symptoms associated with balance disorders. For instance, vestibular suppressants, such as meclizine, can help alleviate vertigo and diminish nausea during acute episodes. These medications can serve as a lifeline for individuals contending with the unpredictable nature of conditions like Meniere’s disease or vestibular neuritis.
Beyond pharmacological interventions, therapeutic approaches such as cognitive-behavioral therapy (CBT) can address the psychological impacts of balance disorders. Many individuals experience anxiety and fear stemming from their symptoms, which can further exacerbate balance difficulties. Through therapy, individuals can learn coping strategies that empower them to manage their symptoms more effectively and regain control over their lives.
Understanding how ear conditions affect balance allows patients and healthcare providers to adopt a proactive treatment approach. By addressing both the physical symptoms and the emotional consequences, individuals can cultivate resilience and improve their overall well-being.
Engaging in Vestibular Rehabilitation for Improved Balance
Vestibular rehabilitation is a specialized form of physical therapy aimed at enhancing balance and reducing dizziness. This therapy often includes customized exercises designed to retrain the brain’s processing of balance information, helping individuals regain their equilibrium and confidence.
Exercises may encompass gaze stabilization techniques, balance training, and habituation strategies, all tailored to an individual’s specific needs and capabilities. For instance, someone who is learning to walk again after a vestibular event may engage in progressive exercises that gradually increase in difficulty, fostering confidence in their balance.
The global perspective on vestibular rehabilitation highlights the importance of access to trained professionals. In some areas, physical therapists specializing in vestibular disorders may be limited, underscoring the need for enhanced education and training opportunities worldwide. By understanding how ear conditions affect balance, communities can advocate for improved access to rehabilitation services, ultimately benefiting those affected by balance disorders.
Considering Surgical Interventions for Severe Conditions
In certain instances, surgical interventions may be necessary to address severe ear conditions impacting balance. Procedures such as labyrinthectomy or stapedectomy can alleviate symptoms and restore function for individuals suffering from debilitating balance disorders. While surgery carries inherent risks, it can also provide substantial relief and improve quality of life for many individuals.
The decision to pursue surgery often involves careful consideration of the associated risks and benefits, along with a thorough understanding of the individual’s overall health and lifestyle. For those residing in regions with limited surgical options, exploring non-invasive alternatives may be crucial for effective symptom management.
Recognizing how ear conditions affect balance can guide individuals in making informed decisions regarding their treatment options. By engaging in open discussions with healthcare providers, patients can explore a range of interventions that align with their health needs and personal preferences.
Implementing Lifestyle Modifications for Better Balance Management
Lifestyle modifications play a pivotal role in managing balance disorders. Simple changes, such as establishing fall prevention strategies within the home, can significantly reduce the risk of accidents. This may involve removing tripping hazards, enhancing lighting conditions, and ensuring access to assistive devices when necessary.
Additionally, dietary adjustments may prove beneficial for individuals with specific ear conditions. For instance, those diagnosed with Meniere’s disease may be advised to limit salt intake to help manage fluid retention in the inner ear. Understanding the relationship between diet and ear health empowers individuals to take proactive measures in controlling their symptoms.
The broader implications of how ear conditions affect balance emphasize the significance of adopting a holistic approach to treatment. By integrating lifestyle changes alongside medical interventions, individuals can create a comprehensive strategy that enhances their overall well-being and fosters resilience against balance issues.
The Role of Assistive Devices in Enhancing Stability
Assistive devices can provide essential support for individuals facing balance disorders. Tools such as canes, walkers, and mobility scooters can significantly enhance stability, allowing individuals to navigate their environment with greater confidence. Furthermore, hearing aids can improve auditory input, which is vital for maintaining balance in various settings.
In many cultures, the use of assistive devices can carry a stigma, leading individuals to avoid seeking necessary support. Raising awareness about the benefits of these devices can help alleviate this stigma, encouraging individuals to embrace tools that enhance their quality of life and independence.
By understanding how ear conditions affect balance, communities can foster an inclusive environment that supports individuals with balance disorders, ultimately promoting autonomy and improving overall quality of life.
Effective Prevention and Management Strategies for Balance Disorders
Preventing and managing balance disorders related to ear conditions necessitates a proactive approach. By concentrating on ear health maintenance, lifestyle modifications, and safety measures, individuals can significantly diminish their risk of developing balance issues.
Prioritizing Ear Health Maintenance
Maintaining good ear health is essential in preventing balance disorders. Regular check-ups with an audiologist or an ear, nose, and throat (ENT) specialist can help identify potential issues before they escalate into more severe conditions. Global awareness and education about ear health should be a priority, as many individuals may be unaware of the importance of routine screenings.
Additionally, practicing good hygiene is vital in preventing ear infections that could lead to balance issues. Simple measures, such as frequent hand washing and avoiding exposure to loud noises, can protect ear health and thus preserve balance.
Understanding how ear conditions affect balance empowers individuals to take charge of their ear health proactively. By emphasizing preventive measures, individuals can reduce the likelihood of developing balance disorders and improve their overall quality of life.
Adopting Lifestyle Adjustments for Better Balance
Lifestyle adjustments can significantly influence the management of balance disorders. Individuals may benefit from adopting healthier habits, such as regular physical exercise and a balanced diet, which can improve physical fitness and overall well-being.
Avoiding substances that could worsen dizziness, such as alcohol, caffeine, and tobacco, is also crucial. These substances can interfere with the vestibular system’s functionality, leading to exacerbated symptoms for those with existing balance disorders.
By understanding how ear conditions affect balance, individuals can make informed lifestyle choices that promote better ear health and minimize the risk of balance issues.
Implementing Safety Measures to Prevent Falls
Implementing practical safety measures within home and community environments can significantly mitigate the risk of falls among individuals with balance disorders. Simple modifications, such as installing handrails, improving lighting conditions, and utilizing non-slip mats, can enhance safety and boost confidence when navigating everyday surroundings.
Community awareness programs play a vital role in educating the public about fall prevention strategies. By fostering a culture of safety, communities can effectively support individuals facing balance challenges, enabling them to engage with their surroundings with greater assurance.
Understanding the broader implications of how ear conditions affect balance can encourage individuals and communities to take collective action in promoting safety and minimizing fall risks.
Seeking Timely Medical Interventions for Balanced Health
Promptly seeking medical interventions can effectively treat the underlying causes of balance disorders and enhance overall ear health. This may involve consultations with specialists, personalized treatment plans, and ongoing symptom monitoring to ensure optimal care.
In regions with limited access to healthcare, advocating for improved services becomes increasingly important. Recognizing the need for comprehensive care empowers individuals to seek the support they deserve, ultimately leading to better management of balance disorders.
By acknowledging how ear conditions affect balance, both patients and healthcare providers can take proactive steps toward maintaining ear health and preventing balance issues, thereby enhancing the quality of life for individuals globally.
The Broader Impact of Balance Disorders on Daily Life
The effects of ear conditions that influence balance extend beyond physical symptoms, permeating various facets of daily life and affecting work, social interactions, and overall well-being.
Challenges in Work and Productivity Due to Balance Disorders
Individuals dealing with balance disorders often encounter significant challenges within the workplace. The unpredictable nature of dizziness and unsteadiness can hinder productivity, making it difficult to concentrate or complete tasks efficiently. For example, a person with Meniere’s disease may find it challenging to participate in meetings or engage in collaborative projects due to the fear of an episode occurring.
In today’s competitive job market, maintaining productivity and job performance is vital for career advancement and financial stability. Thus, understanding how ear conditions affect balance can foster empathy among employers and colleagues, paving the way for more supportive work environments.
Accommodations such as flexible work arrangements, modifications to the physical workspace, or access to assistive devices can significantly enhance the ability of individuals with balance disorders to thrive professionally. By creating inclusive workplace cultures that acknowledge the challenges posed by ear conditions, organizations can empower employees to contribute meaningfully and confidently.
Frequently Asked Questions about Balance Disorders
What symptoms are commonly associated with ear-related balance disorders?
Common symptoms can include dizziness, vertigo, lightheadedness, nausea, and feelings of unsteadiness, which significantly increase the risk of falls and injuries for those affected.
In what ways do ear infections impact balance?
Ear infections can disrupt the vestibular system by causing inflammation and fluid accumulation, leading to dizziness and various balance challenges.
Can you explain Meniere’s disease and its effects on balance?
Meniere’s disease is characterized by episodes of vertigo, hearing loss, and tinnitus due to fluid accumulation in the inner ear, severely disrupting balance.
What methods are used to diagnose balance disorders?
Balance disorders can be diagnosed through a combination of hearing tests, vestibular function tests, and imaging studies that assess the inner ear structures and their functionality.
What types of treatments are available for managing balance disorders?
Treatment options include medications, vestibular rehabilitation, surgical interventions, and lifestyle modifications aimed at effectively managing symptoms and improving quality of life.
Can lifestyle changes contribute to balance disorder management?
Yes, adopting lifestyle changes such as engaging in regular exercise, adjusting dietary habits, and implementing fall prevention strategies can significantly enhance balance and overall health.
How do assistive devices aid those with balance disorders?
Assistive devices like canes, walkers, and mobility scooters can significantly improve stability and mobility, enabling individuals to navigate their environments more confidently.
What are the effects of aging on balance?
Aging can lead to a decline in vestibular system function, increasing the likelihood of balance disorders and falls among older adults.
What steps should I take if I experience dizziness or balance issues?
Consult a healthcare professional for a thorough evaluation and diagnosis, as timely intervention can address underlying ear conditions and enhance balance.
Is there a correlation between hearing loss and balance disorders?
Yes, hearing loss is often linked with balance disorders, as both conditions are frequently associated with dysfunction in the inner ear structures responsible for maintaining equilibrium.
Explore our journey on X!
The post Ear Conditions and Balance: Exploring the Connection appeared first on The Microsuction Ear Wax Removal Network.